This superb book by Dr. Neil Nathan is a must-read for anyone suffering from mold toxicity, Lyme disease, multiple chemical sensitivities, chronic environmental illness, fibromyalgia, or myalgic encephalomyelitis/chronic fatigue syndrome. These difficult-to-treat diseases, which are often ignored or dismissed by mainstream medical practitioners, present a challenge to any physician, but it is a challenge that Dr. Nathan meets with in-depth knowledge, compassion, and common sense. In addition to the above diseases, Dr. Nathan also discusses the important role of mast cell activation, porphyria, and carbon monoxide, the three “elephants in the room.” His discussion of mast cell activation syndromes, which he finds in half of his patients suffering from unusual sensitivities, is particularly enlightening. He not only presents symptoms and signs to look for, but how MCAS is diagnosed and treated.
Dr. Nathan brings his decades of experience to bear by explaining how toxins can interact to produce a multiplicity of disease states simultaneously. His clear and concise explanation for how environmental diseases become chronic is the best I have ever read. In some individuals, toxins are not eliminated through normal channels. Instead, the toxins, once they are attached to bile, are recycled, sent back to the liver when the bile is reabsorbed in the large intestine. This would account for why people with exposure to mold, for example, do not recover after a single course of treatment.
People with any of the illnesses covered in this book will be delighted to find detailed descriptions of how Dr. Nathan and other experts in this field treat these diseases. Not only does Dr. Nathan offer a treatment blueprint for each disease, he provides many additional resources, as well as direct commentary by expert physicians. His bottom line is that it is not enough to kill infections, or rely on strict avoidance. Toxins must be safely removed. The underlying theme, namely chronic inflammation, is addressed in this context. Dr. Nathan’s chapters on” rebooting” as a model for treatment and healing are a goldmine for people seeking an effective long-term treatment strategy.
One of the most valuable takeaways from this book is Dr. Nathan’s sensible approach. Dr. Nathan takes “First, do not harm” seriously. Patients with environmental illnesses can be exquisitely sensitive, which means treatments must be started at miniscule doses, and proceed slowly. If a patient feels worse, stop. Why insist that a patient “push through” if it only leads to increased symptoms? This is so sensible, and so obvious, I am left wondering why more physicians don’t adopt a more gradual approach to treating environmental diseases.
Dr. Nathan’s conversational writing style makes this book a pleasure to read, despite the complexity of the topic. He increases the accessibility to lay readers by including helpful diagrams and graphics that convey information visually, as well as side notes that neatly summarize points. This is a book to keep by your bedside. You will want to refer to it often.
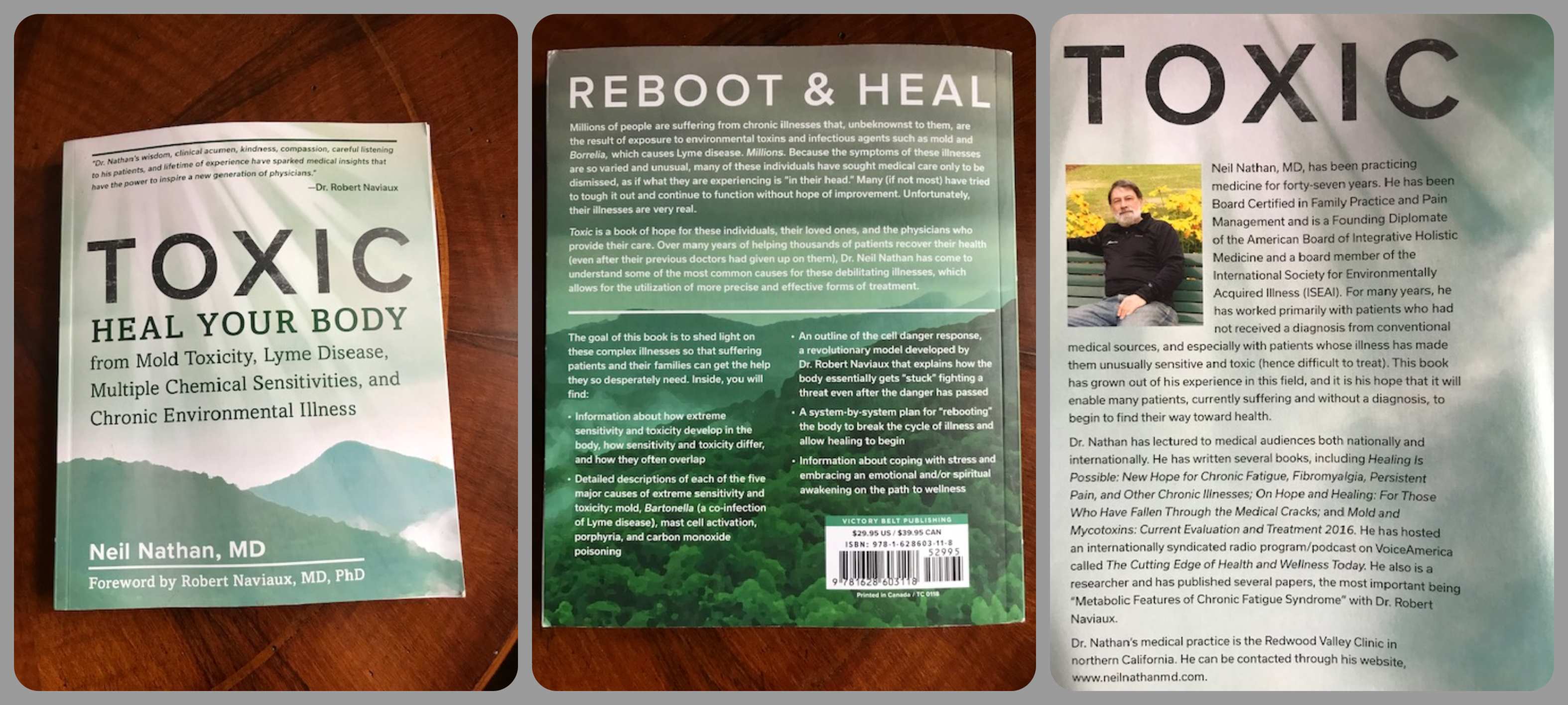
Available on Amazon and Barnes&Noble.