Patients with ME/CFS commonly experience one or more conditions that may appear simultaneously with ME/CFS, occur prior to a diagnosis of ME/CFS, or appear years later. Some of these, like fibromyalgia, have symptoms that are so similar to ME/CFS that it is hard to distinguish between them. Others, like migraines, may only appear in a subset of ME/CFS patients.
When conditions overlap, it is often difficult to make an accurate diagnosis. Some patients discover years after their ME/CFS diagnosis that they have a different illness entirely. For these patients, years may have been lost while their actual illness remained untreated.
If you have symptoms of easy fatigability, exercise intolerance, painful joints or muscles, or sleep disturbance, do not automatically assume that you have ME/CFS. These symptoms are common to a number of ailments.
ILLNESSES WITH SYMPTOMS SIMILAR TO ME/CFS
Patients with the following illnesses can be misdiagnosed with ME/CFS. These illnesses may be difficult to detect in their early stages, and will require a specialist for a proper diagnosis. All of these illnesses, as well as others, have been missed by physicians who have treated patients misdiagnosed with ME/CFS.
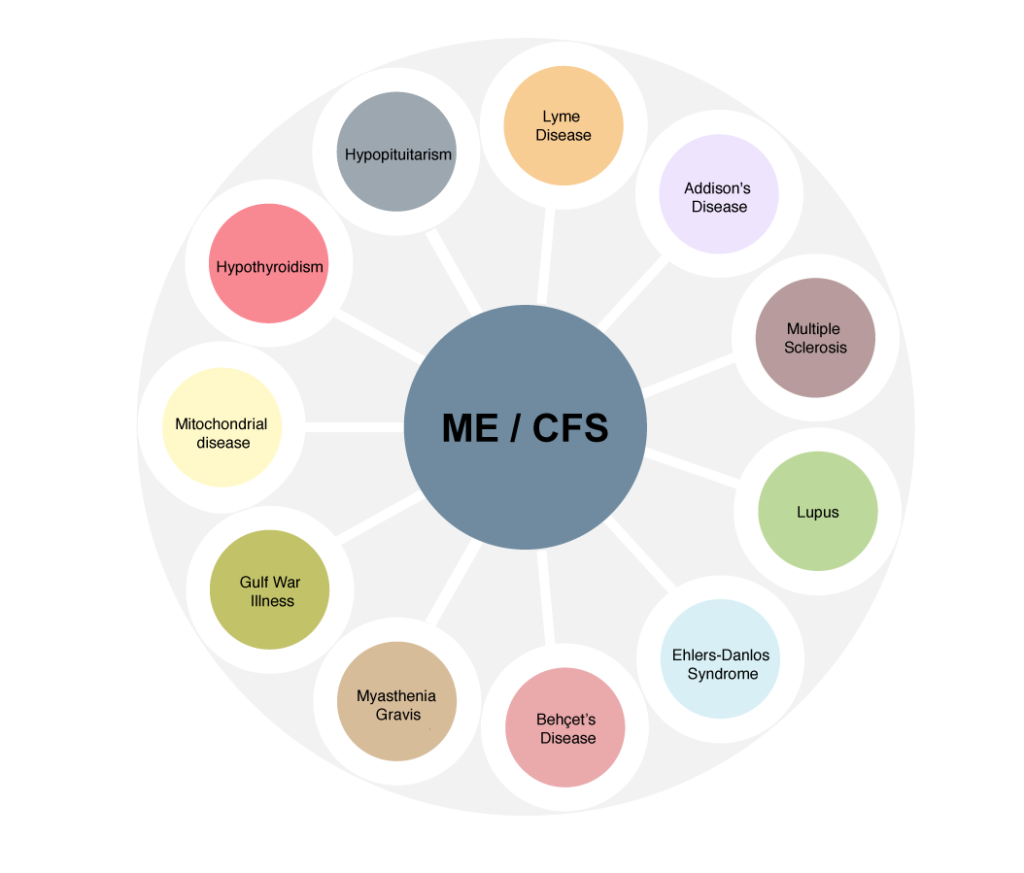
- Multiple Sclerosis – Because Multiple Sclerosis initially presents with profound fatigue, up to one-third of Americans with early MS have been misdiagnosed with CFS (Berger et al.) If you have any neurological symptoms suggestive of MS – numbness, tingling, dizziness, inappropriate sensations (cold objects feel hot) – see your doctor.
- Ehlers-Danlos Syndrome – EDS is a genetic connective tissue disorder that produces pain, fatigue, unrefreshing sleep, and cognitive impairment – all of which are common symptoms of ME/CFS. Joint hypermobility is the cardinal symptom of EDS.
- Lyme Disease – Lyme disease is a bacterial infection caused by the bite of an infected tick of the species Ixodes. The CDC acknowledges that there are over 400,000 new cases of Lyme disease each year, making it the fastest growing tick-borne infection in the U.S. While Lyme disease is usually a short-term infection, it may become chronic in up to 30% of patients. The symptoms of chronic Lyme disease are virtually identical to those of ME/CFS. If you develop symptoms typical of ME/CFS and live in a Lyme endemic area, be sure your doctor tests you for Lyme disease. You may have to be tested several times, as the Lyme disease tests currently in use are notoriously unreliable. The standard treatment for Lyme is antibiotics.
- Behçet’s Disease – Behçet’s disease (pronounced beh-SHETS), also called Behçet’s syndrome, is a rare autoimmune disease that causes inflammation in blood vessels. Canker sores or ulcers in the mouth are a hallmark symptom of the disease, but inflammation can also occur in parts of the eye, joints, GI tract, brain and spinal cord. Because patients with Behçet’s disease experience profound fatigue they are often misdiagnosed with CFS. If you notice sores in your mouth or on your body, be sure to mention these to your doctor.
- Hypopituitarism – Hypopituitarism or “empty sella syndrome” is a condition in which the pituitary gland shrinks. The symptoms overlap those of ME/CFS: profound fatigue, headaches, pain, and weakness. If symptoms appear after a brain injury or concussion, surgery, or an infection involving the central nervous system, an MRI should be performed, along with tests to measure pituitary hormones.
- Mitochondrial Disease – Mitochondrial disease is a genetic disorder that affects the functioning of the mitochondria – the body’s source of cellular energy. The primary symptoms are profound fatigue, muscle weakness, loss of coordination, pain, gastro-intestinal problems, and, in children, slow growth. It is passed down through the mother, so if there is any history of those symptoms on the mother’s side, mitochondrial disease should be ruled out. While in most cases mitochondrial disease occurs in children, adult onset of mitochondrial disease is not unknown.
- Myasthenia Gravis – Myasthenia Gravis is an autoimmune disease affecting the voluntary muscles. It is characterized by weakness of arm or leg muscles, double vision, drooping eyelids, and difficulties with speech, chewing, swallowing, and breathing. The weakness may come and go, but over time it will become progressive. If your muscle weakness is your predominant symptom or if it worsens, be sure to see an immunologist.
- Hypothyroidism – Hypothyroidism and Hashimoto’s disease, and autoimmune disease affecting the thyroid gland, are fairly common in the U.S., affecting between 4.6 and 12 percent of the population. Women are more likely than men to develop hypothyroidism, particularly during pregnancy. Because the thyroid regulates the body’s metabolism, the primary symptoms of low thyroid function are fatigue, slowed mental processes, cold intolerance, joint and muscle pain, and sleep disturbance – all of which are common symptoms in ME/CFS patients. If you experience these symptoms, as well as dry hair or hair loss, brittle nails, puffiness in the face or around the eyes, constipation, depression, and weight gain, be sure to have your thyroid checked.
- Lupus – Lupus can damage any part of the body. The most common symptom of early lupus is fatigue. Lupus can also cause joint pain, “brain fog,” light sensitivity, mouth sores, low fevers, and inflammation in organs. A typical feature of lupus is the “butterfly” rash across the top of the cheeks and nose. Lupus symptoms may come and go. Onset can be sudden or insidious. Another form of lupus, drug-induced lupus, occurs after long-term (months to years) daily use of a medication. Once the medication is stopped, symptoms of drug-induced lupus typically disappear completely within six months. Drug-induced lupus does not lead to systemic lupus.
Comorbidities
When an illness or condition is experienced alongside another illness it is called a comorbidity. Comorbidities are so common in the ME/CFS patient population that it is rare to find a patient who does not have several (Aaron et al).
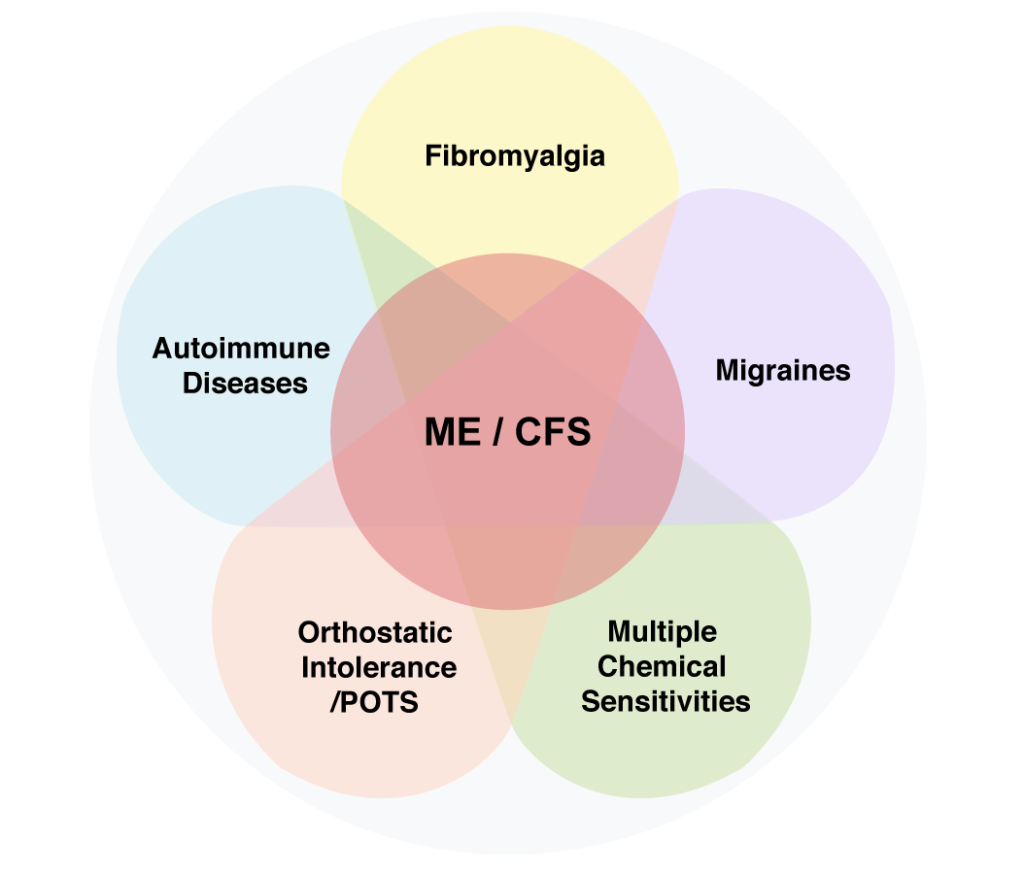
Fibromyalgia
The most common overlapping condition with ME/CFS is fibromyalgia. In ME/CFS dominant patients, the fibromyalgia pain is not constant, but tends to appear when there is an additional injury or infection, such as an accident, a viral infection, or a surgical procedure. Fibromyalgia is a syndrome, with many symptoms in addition to pain. However, if pain is not present, the patient cannot receive a diagnosis of fibromyalgia.
Other related pain syndromes that may occur with ME/CFS are:
- Temporomandibular disorder (TMJ) – A painful condition caused by dysfunction in the jaw joint and the muscles that control jaw movement.
- Chronic pelvic pain – This is a condition experienced by women in which pain is experienced below the navel. Many conditions can lead to chronic pelvic pain, including endometriosis, infections of the ovaries, irritable bowel syndrome and various hormonal irregularities.
- Chronic nonbacterial prostatitis – Experienced by men, and, as with pelvic pain in women, may result from a number of causes, such as bicycle riding, viruses, parasites, and neurological problems.
- Interstitial Cystitis – IC is a painful condition that mimics the symptoms of ordinary cystitis, but without bacterial infection. According to Dr. Larrian Gillespie, author of You Don’t Have to Live With Cystitis, IC is caused by the erosion of the GAG layer, which is the mucous lining that protects the bladder from its contents. Mast cell activation, an immune process, is believed to be the driving force that leads to the erosion of the GAG layer (Theoharides et al).
Autoimmune Disease
It has been proposed that ME/CFS is an autoimmune disorder, because it shares distinctive chemical markers with other autoimmune diseases (Staines et al). Clinicians have observed that a diagnosis of ME/CFS may precede a diagnosis of autoimmune disorder, which means that either the correct diagnosis was initially missed, or that the patient subsequently developed an autoimmune disease. The following are some autoimmune diseases that most frequently occur as comorbidities with ME/CFS.
- Hashimoto’s Disease – Dr. John Richardson noted that among his ME patients, 20% developed Hashimoto’s disease, an autoimmune disease that affects the thyroid. Patients with Hashimoto’s disease often have normal lab results, so the diagnosis may be missed for several years.
- Sjögren’s Syndrome – An autoimmune disease that causes dry mouth and eyes, along with other symptoms
- Lupus – An autoimmune disease that can damage any part of the body (skin, joints, and/or organs inside the body). Lupus is characterized by a distinctive face rash resembling a wolf, from which the disease gets its name.
Migraines
Headaches of a new variety or severity are experienced by upwards of 75% of the patient population according to Dr. Katrina Berne. Some patients suffer from these headaches daily.
The most common variety of headache experienced by ME/CFS patients is migraine, which is found in 60-84% of patients with ME/CFS (Ravindran et al).
Multiple Chemical Sensitivity
Multiple Chemical Sensitivity (MCS) produces a severe reaction to many different kinds of pollutants including solvents, VOC’s (Volatile Organic Compounds), perfumes, petrol, diesel, smoke, and other chemicals. In a five-year study of 690 patients conducted by Dr. Dedra Buchwald, more than 50% of patients with ME/CFS reported having chemical sensitivities. Research conducted by I. R. Bell in 1998 showed a similar percentage. A 2000 study by Jason et al. found that roughly 40% of patients with ME/CFS also met the criteria for multiple chemical sensitivities (MCS).
The symptoms of MCS are wide-ranging and may include burning and stinging eyes, wheezing, breathlessness, nausea, extreme fatigue/lethargy, headache/migraine/vertigo/dizziness, poor memory and concentration, runny nose (rhinitis), sore throat, cough, sinus problems, skin rashes and/or itching skin, sensitivity to light and noise, sleeping problems, digestive upset, and muscle and joint pain.
Orthostatic Intolerance and Postural Orthostatic Tachycardia Syndrome (POTS)
Many, if not most, patients with ME/CFS report problems standing (orthostatic intolerance). Orthostatic intolerance (OI) is a broad classification referring to exaggerated blood pressure and/or heart rate responses that occur when standing up. When a healthy person stands up, the effects of gravity cause about 10-15% of the blood to settle (pool) in the abdomen, legs, and arms. To make up for the reduced amount of blood returning to the heart, the adrenal glands release adrenaline and noradrenaline (epinephrine and norepinephrine), which cause the heart to beat a little faster and blood vessels to constrict.
People with OI have reversed responses to changes in position. When people with OI stand up, they pool a larger amount of blood in regions below the heart. The longer they remain upright, the more blood pools in their abdomen and legs. The adrenal glands respond by releasing more adrenaline and noradrenaline in an attempt to cause constriction of the blood vessels and boost cardiac output.
However, the blood vessels do not constrict enough to ensure increased back flow into the heart, and the heart races. This, in turn, leads to lower blood volume (hypovolemia), which perpetuates the cycle.
The symptoms produced by this loop are fatigue, nausea, light-headedness, heart palpitations, sweating, and sometimes fainting (syncope). The feedback loop that leads specifically to an increased heart rate of 30 bpm (beats per minute) or more when standing is called POTS – postural orthostatic tachycardia syndrome.
According to Dr. Julian Stewart, director of the Center for Hypotension at the New York Medical College, “orthostatic intolerance in most adolescents (and many adults) with CFS appears to be POTS.” OI/POTS is so common in the patient population that Hoad et al. have recommended that the response to standing should be a diagnostic marker for ME/CFS.
FURTHER READING
The Brainstem – Is it THE Pain Conductor in Fibromyalgia? By Cort Johnson
REFERENCES
Aaron , Leslie A,, PhD, MPH,1 Richard Herrell, MS, Suzanne Ashton, BS, Megan Belcourt, Karen Schmaling, PhD, Jack Goldberg, PhD, and Dedra Buchwald, MD.Comorbid Clinical Conditions in Chronic Fatigue: A Co-Twin Control Study. J Gen Intern Med. Jan 2001; 16(1): 24-31. doi: 10.1111/j.1525-1497.2001.03419.x PMCID: PMC1495162
Bell IR, Baldwin CM, Schwartz GE. “Illness from low levels of environmental chemicals: relevance to chronic fatigue syndrome and fibromyalgia.” Am J. Med. 1998 Sep 28;105(3A):74S-82S.
Berger JR, Pocoski J, Preblick R, Boklage S. Fatigue May Be Early Sign of MS. Mult Scler. 2013 Feb 25.
Buchwald, Dedra, MD; Deborah Garrity, MD. “Comparison of Patients With Chronic Fatigue Syndrome, Fibromyalgia, and Multiple Chemical Sensitivities.” Arch Intern Med. 1994;154(18):2049-2053.
Castori M, Morlino S, Celletti C, Celli M, Morrone A, Colombi M, Camerota F, Grammatico P. Management of pain and fatigue in the joint hypermobility syndrome (a.k.a. Ehlers-Danlos syndrome, hypermobility type): principles and proposal for a multidisciplinary approach. Am J Med Genet A. 2012 Aug;158A(8):2055-70. doi: 10.1002/ajmg.a.35483. Epub 2012 Jul 11.
Hoad A, Spickett G, Elliott J, Newton J. “Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome.” QJM. 2008 Dec;101(12):961-5.
Jason LA, Taylor RR, Kennedy CL. “Chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities in a community-based sample of persons with chronic fatigue syndrome-like symptoms.” Psychosom Med. 2000 Sep-Oct;62(5):655-63.
Ravindran MK, Zheng Y, Timbol C, Merck SJ, Baraniuk JN. Migraine headaches in chronic fatigue syndrome (CFS): comparison of two prospective cross-sectional studies.BMC Neurol. 2011 Mar 5;11:30. doi: 10.1186/1471-2377-11-30.
Reynolds GK, Lewis DP, Richardson AM, Lidbury BA. Comorbidity of postural orthostatic tachycardia syndrome and chronic fatigue syndrome in an Australian cohort. J Intern Med. 2014 Apr;275(4):409-17. doi: 10.1111/joim.12161. Epub 2013 Nov 29.
Richardson, John. Enteroviral and Toxin Mediated Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Other Organ Pathologies. CRC Press; 2001.
Schondorf, R., Freeman, R. “The importance of orthostatic intolerance in the chronic fatigue syndrome.” Am J Med Sci. 317: 117-123, 1999.
Staines DR. Is chronic fatigue syndrome an autoimmune disorder of endogenous neuropeptides, exogenous infection and molecular mimicry? Med Hypotheses. 2004;62(5):646-52.
Stewart, Julian. “Orthostatic Intolerance.” In Leonard A. Jason, Patricia A. Fennell, and Renée R. Taylor, eds. Handbook of Chronic Fatigue Syndrome. New Jersey: John Wiley and Sons, 2003.
Theoharides TC, Pang X, Letourneau R, Sant GR. “Interstitial cystitis: a neuroimmunoendocrine disorder.” Ann N Y Acad Sci. 1998 May 1;840:619-34.