 ME/CFS is a syndrome, which means it is characterized by numerous symptoms. Much like autoimmune diseases, ME/CFS symptoms may wax and wane. Some may disappear entirely for months, only to re-appear when a new treatment is initiated, or when the patient contracts a viral or bacterial infection.
ME/CFS is a syndrome, which means it is characterized by numerous symptoms. Much like autoimmune diseases, ME/CFS symptoms may wax and wane. Some may disappear entirely for months, only to re-appear when a new treatment is initiated, or when the patient contracts a viral or bacterial infection.
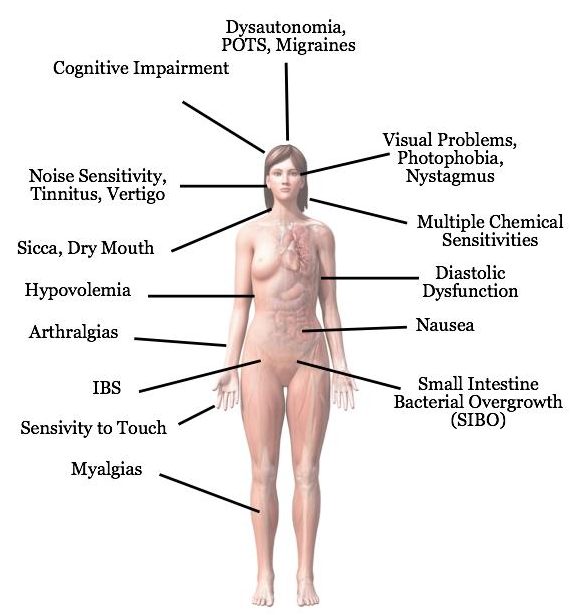
As a “multi-system” disease, ME/CFS affects all major systems in the body, including the immune system, nervous system, and endocrine system. Because these three systems have such far-reaching effects on physiological functions, the list of symptoms caused by alterations in these systems is staggering. Melissa Kaplan has assembled a list of over 200 symptoms reported by patients. Not all of these symptoms are experienced by every patient. However, there are a few that are universal.
Dr. Leonard Jason’s team at De Paul University found that eleven symptoms were sufficient to accurately identify ME/CFS patients. These symptoms were clustered in five areas:
- Profound loss of energy (fatigue)
- Post-exertional malaise of PEM (symptoms worsen after physical or mental exertion)
- Cognitive impairment
- Unrefreshing sleep
- Pain in joints and muscles, as well as headaches
Doctors often refer to the above symptoms as “non-specific” meaning they are common to a number of illnesses. In fact, healthy people also experience fatigue, muscle aches, and insomnia, as well as many other symptoms on the list, but what marks ME/CFS symptoms as unusual is that they worsen after exertion. They are also distinguished by their severity, frequency and duration. ME/CFS symptoms can be incapacitating, they can be experienced daily, and symptoms may last for years.
SYMPTOMS SCALE
Not all patients experience the same severity of illness. As with any other disease, including the common cold, symptoms can be mild, moderate or severe. Patients often rate themselves on a 1-10 scale, with 1 being bedbound, and 10 fully recovered.
In addition, there are three general levels of illness: mild, moderate, and severe.
Mild: Patients are mobile, can care for themselves, do light housework and work part-time, or even full-time with the curtailment of all other activities. Mildly ill patients experience easy fatigability and loss of stamina and must plan their activities carefully.
Moderate: Patients have reduced mobility and are restricted in all activities of daily living. They have usually stopped work or school. Moderately ill patients feel exhausted after activities.
Severe: Patients are unable to do anything without assistance. They spend most of the day in bed and are sensitive to light and noise. Severely ill patients often feel as if they have the flu.
Patients may suffer relapses at any point in the illness. Even mildly ill patients may become severely ill during a relapse.
A HETEROGENEOUS ILLNESS
Doctors are often confused by the wide array of symptoms experienced by patients with ME/CFS, as well as by the fact that not all patients experience all of them. Yet, multiple symptoms are common in any chronic disease. Hypothyroidism has over 300 symptoms, and not all patients experience all of them. The same is true of autoimmune diseases, such as lupus, which affect multiple systems.
A good explanation for why some patients predominantly experience one set of symptoms, while others experience another can be found in genetics.
A 2016 study published in the Journal of Translational Medicine (Paul Billing-Ross et al.) examined mitochondrial DNA in ME/CFS patients. They found that 1) none of the patients showed any evidence of a mitochondrial genetic disease; 2) there was difference in the types of mitochondrial DNA between patients and healthy individuals, and 3) there was no increased susceptibility to ME/CFS among people with different mitochondrial SNPs (single nucleotide polymorphisms, or variations in DNA).
However, the study showed associations of SNPs with certain symptoms and/or their severity. Individuals who carry a particular SNP, for example, are predicted to be at greater risk of experiencing particular types of symptoms once they become ill.
The authors remarked:
“A puzzling aspect of ME/CFS has been the diversity of symptoms and the variation of their severity among different individuals. These differences should not be taken as proof that more than one insult was the initiating factor, nor that different patients have different underlying problems. It remains possible that much of the diversity of the manifestation of the illness results from genetic diversity rather than the existence of multiple fundamental causes.”
ME/CFS Signs and Symptoms Checklist
[ ] Fatigue, characterized as a profound loss of energy
[ ] Worsening of symptoms after physical or mental exertion (post-exertional malaise, or PEM)
[ ] Cognitive function problems
[ ] Attention deficit disorder (inability to concentrate)
[ ] Feeling “spaced out” or “cloudy,” “brain fog”
[ ] Calculation difficulties
[ ] Memory loss
[ ] Spatial disorientation
[ ] Word searching or saying the wrong word
[ ] Sleep disturbance, unrefreshing sleep
[ ] Flu-like malaise, feeling “sick all over”, or “poisoned”
[ ] Sore throat
[ ] Low-grade fever or feeling hot often
[ ] Low body temperature
[ ] Muscle and joint aches with or without “trigger points”
[ ] Headache
[ ] Changes in vision
[ ] Numbness or tingling sensations
[ ] Loss of balance, dizziness
[ ] Unusually vivid dreams, nightmares, or lack of dreams
[ ] Depression
[ ] Anxiety, panic attacks
[ ] Personality changes
[ ] Mood swings
[ ] Difficulty moving the tongue to speak
[ ] Tinnitus (ringing in the ears)
[ ] Paralysis
[ ] Severe muscle weakness
[ ] Difficulty walking
[ ] Blackouts
[ ] Photophobia (light sensitivity), and increased sensitivity to noise, smells, touch
[ ] Alcohol intolerance
[ ] Changes in taste, smell, hearing
[ ] Decreased libido, impotence
[ ] Muscle twitches
[ ] Severe premenstrual syndrome (PMS) or exacerbation of symptoms before and during period
[ ] Weight changes, usually loss followed by gain
[ ] Painful, swollen lymph nodes, especially on the neck and underarms
[ ] Abdominal pain, diarrhea, nausea, gas, irritable bowel
[ ] New allergic reactions to medicines, food, and other substances
[ ] Night sweats
[ ] Heart palpitations
[ ] Uncomfortable or frequent urination
[ ] Rash of herpes simplex or shingles
[ ] Flushing, rash
[ ] Hair loss
[ ] Chest pain
[ ] Dry eyes and mouth (sicca)
[ ] Cough, dry
[ ] Canker sores
[ ] Cold hands and feet
[ ] Shortness of breath
[ ] Temperature and weather sensitivity
[ ] Symptoms worsen when standing up (orthostatic intolerance)
[ ] Seizures, usually petit mal, but sometimes grand mal
Reprinted with the kind permission of Katrina Berne. Copyright © 2014 Katrina Berne
FIVE CARDINAL SYMPTOMS
FATIGUE
The best known symptom of ME/CFS is a persistent loss of energy that physicians call “fatigue.” However, the profound loss of energy experienced by ME/CFS patients is nothing like the fatigue most people experience at the end of a long day or following a strenuous workout. It cannot be relieved by rest or sleep. In fact, patients may awaken feeling just as fatigued as they did before they went to sleep, if not more so.
The Centers for Disease Control (CDC) describes the fatigue of ME/CFS as “severe, incapacitating, and all-encompassing.” It is so pervasive that it significantly limits the ability to work, go to school, participate in social activities, and attend to personal needs. The most severe cases of “fatigue” can leave patients housebound or bedridden.
The best way to portray the loss of energy that patients experience is in their own words. Meg, a British blogger with ME/CFS, asked fellow sufferers to explain “what it is really like to have ME.” They responded with graphic descriptions.
- your body is ‘running on empty’ and there’s no way of filling your tank back up
- living in the body of an ill 85-year-old, even at age 15
- every tiny task takes a mammoth amount of effort, as your limbs feel like they’ve been filled with concrete and you don’t have the strength to lift them
- your body is screaming as you push it from bed to bathroom, like it’s the last half mile climbing a 10,000ft mountain
- your body is a faulty phone battery that’s always about to die, and you have no charger
- you’re completely drained of all energy and ‘life’
What is clear from these descriptions is that “fatigue” is too vague a term to adequately characterize what is experienced by patients. It is also clear that several different mechanisms are involved, producing several different types of fatigue.
Causes of fatigue
Neurological illnesses such as multiple sclerosis and Parkinson’s disease also present with profound fatigue, as do autoimmune diseases and hypothyroidism. All three systems – immune, endocrine, and CNS – have been proposed as the cause of the fatigue found in ME/CFS. In addition, fatigue is also characteristic of mitochondrial disease. Because ME/CFS affects all systems as well as mitochondrial function, it is likely that the fatigue experienced by patients can be attributed to malfunctions in all of the above.
POST-EXERTIONAL MALAISE (PEM)
One of the hallmark symptoms of ME/CFS is post-exertional malaise (PEM), a phenomenon in which the illness is exacerbated by exertion of any kind, mental or physical. The exacerbation usually begins 12 to 72 hours after the exertion and requires an extended period of recovery, during which a severely ill patient may be completely unable to function. Post-exertional malaise is also experienced by patients with Lyme disease, an illness that has a strong neurological component.
Patients sometimes refer to PEM as “post-exertional collapse” or “post-exertional relapse” depending on the severity of the symptoms. In patients who are severely ill, even minimal activity can provoke PEM. The more recovered the patient, the more activity it takes to produce PEM. In patients who are mildly ill, strict adherence to pacing can enable them to avoid PEM altogether. (Pacing does not help patients who are bedridden, and has limited value for those who are housebound.)
Patients describe PEM as being “hit by a truck,” “having a “hangover and the flu, while having to run a marathon,” “like death.” In moderately to severely ill patients, all symptoms may be exacerbated, including cognitive problems, flu-like symptoms (swollen glands, sore throat), pain, orthostatic intolerance, etc.) Mildly ill patients may merely feel an increase in exhaustion and achiness.
Exertion, especially physical exertion, beyond a patient’s limits is dangerous. Putting strain on an ill body not only causes an exacerbation of the illness, it can lead to a permanent deterioration. In that sense, PEM is not just a symptom, it is a warning. But because PEM is delayed, and not even the patient may realize that he or she has passed the limit, the warning may come too late. Doctors should be advised that “pushing” their ME/CFS patients will only do them harm.
(See: The Significance to ME/CFS of the Landmark Change to the UK Law on Consent on changes to British law regarding a doctor’s liability concerning advice that might potentially harm a patient.)
Causes of PEM
PEM is not covered in medical school curricula, but exercise intolerance is. Cardio-pulmonary diseases are good examples of diseases that produce exercise intolerance. In congestive heart failure, for instance, the heart simply cannot pump enough blood to keep the body supplied with sufficient oxygen to maintain itself. It has been proposed that PEM in ME/CFS patients may be due to a similar mechanism.
VanNess and colleagues found that during a two-day cardio-pulmonary exercise test (CPET), oxygen uptake in ME/CFS patients diminished, unlike healthy controls. Reduced oxygen uptake could easily lead to increased symptoms, as well as affecting all systems in the body.
Diastolic dysfunction has also been implicated in PEM. Peckerman et al. found that in ME/CFS patients there was reduction in the heart’s ability to fill after pumping blood out through the vascular system (diastolic dysfunction). Peckerman’s group found that the severity of PEM, as well as flu-like symptoms, correlated with the degree of cardiac insufficiency.
Alterations in the microbiome may also contribute to PEM. A 2015 study by Shukla and colleagues found changes in the composition of intestinal flora in ME/CFS patients after exercise that were not found in healthy controls. In addition, clearance of bacteria from the blood was delayed in ME/CFS patients following exercise compared to controls. The authors speculated that “increased bacterial translocation following exercise in ME/CFS patients that may account for the profound post-exertional malaise experienced by ME/CFS patients.”
COGNITIVE IMPAIRMENT
The inability to think can be devastating for ME/CFS patients. Not only do patients lose jobs and sacrifice hard-won careers to “brain fog,” they may also find themselves unable to read a book or follow the plot of a movie. Unlike some of the more obvious physical symptoms, the loss of cognitive ability casts a long shadow over patients. The effort to retrieve common words, forgetfulness, and constant errors are embarrassing, and often lead patients to believe that along with loss of physical stamina and strength they have lost their intelligence.
In fact, patients who contract ME/CFS have been known to lose IQ points. A former clinical psychologist reported a drop of 20 points after falling ill (Social Security Disability Application). Dr. Shiela Bastien and colleagues conducted repeated IQ tests and found “definite shifts in intellectual functioning during the course of the illness.”
While adults suffer from embarrassment, and even shame, over losing mental function, adolescents may be even more greatly affected. A Dutch study (Linde Nijhof et al.) found that IQ scores of CFS adolescents were lower than the IQ scores of healthy peers with an equivalent school level. For teens, whose self-image largely depends on what others think of them, becoming “slow” in high school can create long-lasting harm. While younger children can quickly catch up on studies once they have recovered, teens may develop a self-concept that they are “lazy” or “dumb” that can become self-perpetuating.
Some of the cognitive problems reported by patients are:
- Becoming lost in familiar locations when driving
- Difficulty with simple calculations (e.g., balancing checkbook)
- Difficulty expressing ideas in words
- Difficulty moving your mouth to speak
- Difficulty making decisions
- Difficulty following directions while driving
- Difficulty remembering names of objects
- Difficulty remembering names of people
- Difficulty recognizing faces
- Difficulty following simple written instructions
- Difficulty following complicated written instructions
- Difficulty following simple oral (spoken) instructions
- Difficulty following complicated oral (spoken) instructions
- Difficulty integrating information (putting ideas together to form a complete picture or concept)
- Difficulty putting tasks or things in proper sequence
- Difficulty paying attention
- Difficulty following a conversation when background noise is present
- Difficulty making and/or retrieving memories (long/short-term memory deficits)
- Difficulty understanding what you read
- Easily distracted during a task
- Feeling too disoriented to drive
- Forgetting how to do routine things
- Forgetting the use of common objects (such as, what to do with the shampoo when you are
- standing in the shower)
- Forgetting how to get to familiar places
- Impaired ability to concentrate
- Losing your train of thought in the middle of a sentence
- Losing track in the middle of a task (remembering what to do next)
- Poor judgment
- Switching left and right
- Slowed and/or slurred speech
- Stuttering; stammering
- Transposition (reversal) of numbers, words and/or letters when you speak and/or speak
- Word-finding difficulty
- Using the wrong word
- Inability to multi-task
Mental tasks, especially those requiring extended concentration or multi-tasking, may also produce PEM. The brain uses enormous amounts of ATP, so it is not surprising that intellectual effort should result in a net deficit in energy production. The addition of diastolic dysfunction and low blood volume to mitochondrial impairment combine to form a “perfect storm” in which the brain suffers the effects of hypoxia.
PAIN
Not all ME/CFS patients experience severe pain, but almost all experience some form of pain, whether it be headaches, intestinal cramps, or general achiness. The most common type of pain experienced by patients is muscle and joint pain which may rove. It is unusual for patients to experience prolonged pain in a single muscle or joint, however prolonged body-wide pain is not unknown.
When pain predominates, a physician may make the diagnosis of fibromyalgia. There is a great deal of overlap in the symptoms of these two illnesses, making dual diagnoses relatively common. Both illnesses feature fatigue, both produce sleep disorders and “brain fog,” and neither has a cure. Despite overlapping symptoms, the illnesses are not identical, and treatments differ.
Pain can be of any type: dull, aching, shooting, piercing, burning, stabbing, throbbing. Patients have reported all of these, as well as unusual sensitivity to heat, cold, and pressure. The presence of unusual pain perception indicates nervous system involvement. The nervous system can generate pain through efferent pathways. It can also amplify pain perception through afferent pathways which are mediated via the dorsal root ganglia in the spine.
In severely ill patients, symptoms such as pain, hypersensitivity to sound, light and touch predominate. Inflammation in the dorsal root ganglia could account for these symptoms. In 2006, a young British woman, Sophia Mirza, died of CFS. When her spine was autopsied, 80% of the dorsal root ganglia of her spine were found to be damaged. The pathologist stated that there was “inflammation in the basal root ganglia” supporting his concept of ME as an inflammatory disease of the brain and spine.
In patients with a high degree of pain, inflammation may be the underlying cause.
SLEEP DISORDER
Most ME/CFS specialists will not make the diagnosis if a patient reports normal, restful sleep. Patients with ME/CFS wake up tired. This is referred to as “unrefreshing sleep.”
While the term “unrefreshing sleep” captures the outcome of sleep disorders, it does not cover the many avenues that lead to feeling exhausted upon waking. Patients with ME/CFS typically experience several types of sleep disorder concurrently or consecutively. It is not unusual for a single patient to have experienced all of them.
- Hypersomnia – sleeping too much (this is common among children and adolescents). At its most severe patients may sleep virtually round the clock.
- Insomnia – typically, patients have problems initiating and maintaining sleep (DIMS).
- Phase Shifting – Dr. John Richards reported that among his ME patients, many could not fall asleep until dawn. He called this “owl syndrome.”
- Sleep apnea – cessation of breathing during sleep. Dr. Paul Cheney reports that sleep apnea is common in his patients.
- Light Sleep – patients remain in a state of light sleep without entering into deep sleep.
- Frequent waking – fragmented sleep is the norm among patients with ME/CFS. Sometimes these interruptions may last for hours, but oftentimes patients may not even be aware that they are waking. Microbursts of alpha waves can wake a patient for a few seconds. While the sleeper may not remember these brief interruptions, they diminish overall quality of sleep and can result in unrefreshing sleep. Alpha wave intrusions are common in autoimmune diseases.
- Hypnagogic Sleep – a state of being half awake and half asleep. Hypogogic sleep can be exacerbated by sleeping pills.
- Dysania – a period lasting one to two hours after awakening in which a person simply cannot get out of bed.
- Myoclonus – involuntary jerks (myoclonus) of the arms, legs, or entire body.
- Dreams and Nightmares – Nightmares are a common early symptom in people with CFS/ME, as are vivid, disturbing, thematic dreams. Conversely, many people also experience a complete lack of dreams, or a sense that their dreams are vague and disjointed. This state of dreamlessness may last for months.
- Night Sweats – excess sweating at night is typical of the initial or acute stages of ME/CFS (or relapse). Night sweats can be caused by immune system activation, hormonal imbalances (typically during menopause), and low blood sugar.
- Restless legs – uncomfortable sensations in the legs that result in a strong desire to move or kick. Getting out of bed and standing up can halt restless legs, but it can also wake patients up completely. It helps to place a rolled up towel under the small of the back, or to sleep with back support if you sleep on your side.
There are many causes for sleep disorders in ME/CFS patients – hormonal swings, endocrine dysfunction (such as low thyroid), blood sugar drops, bradycardia (slowed heart rate), secondary infections – but the underlying mechanism is neurological.
The nervous system is roughly divided into two components: sympathetic and parasympathetic. While the sympathetic nervous system is associated with waking activities, such as the “fight or flight” response, the parasympathetic controls passive functions such as digestion and sleep. These two systems, sympathetic and parasympathetic, act like a seesaw. When one is up the other is down. Sleep disturbances, while the causes may vary widely, all revolve around sympathetic dominance at night, when the parasympathetic nervous system should be in full swing.
FURTHER READING
In Their Own Words: Chronic Fatigue Syndrome and Fibromyalgia Patients Describe Their Symptoms
Taking heart. Part 2: The heart and circulation in ME/CFS – This is the second article by Dr Eleanor Roberts looking at how abnormalities in the heart and circulation may be involved in some of the symptoms of ME/CFS. Read part 1 here, which provides an introduction to the heart, blood vessels and how they are regulated.
The Chronic Illness Survey Adventure (Symptom Cluster Characterization in Complex Chronic Disease) is a survey-based study to probe more deeply into ME/CFS, Long COVID, POTS, hEDS, and MCAS.
Post-Exertional Symptom Exacerbation (PESE). ME/CFS South Australia Inc provides a comprehensive description of post-exertional malaise, assessment, and management.
What Is Post-Exertional Malaise? Bateman-Horne center information sheet.
Heart Rate Variability Handout. Heart Rate Variability (HRV) is the difference in time between heartbeats. It indicates how your autonomic nervous system functions and can provide valuable information to help prevent post-exertional malaise (PEM/PESE).
Like every well-equipped car has jumper cables, we encourage patients and loved ones to keep an illness crash care kit in the car. Read Appendix 1 of the ME/CFS Crash Survival Guide here: https://batemanhornecenter.org/crash-care-kit-essentials/
Why the 10-Minute NASA Lean Test? Dr. Bateman breaks down the findings of the last three published studies on orthostatic intolerance conducted at BHC to explain why the 10-Minute NASA Lean Test is an effective and accessible way to assess orthostatic intolerance.
REFERENCES
Autonomic Dysfunction. Webpage from ME/CFS South Australia. https://mecfssa.org.au/resources/autonomic-dysfunction
Bastien. D.G. Watson, D. Peterson. IQ Abnormalities Associated With Chronic Fatigue Syndrome In Repeated Wais-R Testing. Paper presented at The First World Congress on Chronic Fatigue Syndrome And Related Disorders . Brussels, November 9-11, 1995. http://www.ncf-net.org/conference/firstwoldabstracts.htm
Paul Billing-Ross, Arnaud Germain, Kaixiong Ye, Alon Keinan, Zhenglong Gu, and Maureen R. Hanson. Mitochondrial DNA variants correlate with symptoms in myalgic encephalomyelitis/chronic fatigue syndrome. J. Translational Medicine. 2016, 14:19 http://www.translational-medicine.com/content/14/1/19
Hanson, Maureen. Mitochondrial DNA and ME/CFS: A Guide to the Hanson Lab’s 2016 JTM Publication. http://hansonlab.org/research/cfs_me/mitochondria/
Kristin Filler, Debra Lyon, James Bennett, Nancy McCain, Ronald Elswick, Nada Lukkahatai, Leorey N. Saligan. Association of mitochondrial dysfunction and fatigue: A review of the literature. BBA Clinical, Elsevier, Volume 1, June 2014, Pages 12–23. http://www.sciencedirect.com/science/article/pii/S221464741400004X
Georgiades E, Behan WM, Kilduff LP, Hadjicharalambous M, Mackie EE, Wilson J, Ward SA, Pitsiladis YP. “Chronic fatigue syndrome: new evidence for a central fatigue disorder.” Clin Sci (Lond). 2003 Aug;105(2):213-8. http://www.ncbi.nlm.nih.gov/pubmed/12708966 (Abstract)
Inquest into the Death of Sophia Mirza. http://www.investinme.org/Article-050%20Sophia%20Wilson%2001-RIP.HTM
Jackson ML; Bruck D. Sleep abnormalities in chronic fatigue syndrome/myalgic encephalomyelitis: a review. J Clin Sleep Med 2012;8(6):719-728. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3501671/
Jason, L. A., Evans, M., So, S., Scott, J., & Brown, A. (2015). Problems in defining post-exertional malaise. Journal of prevention & intervention in the community, 43(1), 20–31. https://doi.org/10.1080/10852352.2014.973239 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295644/
MASTER Symptom List for CFS, FMS, CMP & Lyme Disease. Melissa Kaplan, The Carousel Network, May-June 2003. http://www.anapsid.org/cnd/files/mastersymptomlist.pdf
Memory Loss and M.E./CFS/CFIDS. http://www.oocities.org/hotsprings/1496/cfs17.htm
Linde N. Nijhof,Sanne L. Nijhof,Gijs Bleijenberg,Rebecca K. Stellato,Jan L. L. Kimpen,Hilleke E. Hulshoff Pol,Elise M. van de Putte. The impact of chronic fatigue syndrome on cognitive functioning in adolescents. Eur J Pediatr. DOI 10.1007/s00431-015-2626-1, 17 August 2015. http://www.ncbi.nlm.nih.gov/pubmed/26334394 (Abstract)
Orthostatic intolerance. (Useful article from ME/CFS South Australia)
Arnold Peckerman, PhD; John J. Lamanca, PhD; Kristina A. Dahl, MD; Rahul Chemitiganti, MD; Bushra Qureishi, MD; Benjamin H. Natelson, MD. Abnormal Impedance Cardiography Predicts Symptom Severity in Chronic Fatigue Syndrome. Am J Med Sci 2003;326(2):55–60. https://pubmed.ncbi.nlm.nih.gov/12920435/
Roberts, Eleanor, MD. Brain fog. Part 1: An introduction to cognitive function. ME Research UK.
Roberts, Eleanor, MD. Brain fog. Part 2: Cognitive function and ME/CFS. ME Research UK.
Shukla SK, Cook D, Meyer J, Vernon SD, Le T, Clevidence D, et al. (2015) Changes in Gut and Plasma Microbiome following Exercise Challenge in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). PLoS ONE 10(12): e0145453. doi:10.1371/journal.pone.0145453 http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0145453
Social Security Disability Application. http://www.cfids-me.org/socsec.html
Tanaka M, Mizuno K, Tajima S, Sasabe T, Watanabe Y. “Central nervous system fatigue alters autonomic nerve activity.” Life Sci. 2009 Feb 13;84(7-8):235-9 http://www.ncbi.nlm.nih.gov/pubmed/19100749 (Abstract)
VanNess, JM, Snell, C, & Stevens, S. (2007) Diminished Cardiopulmonary Capacity During Post-Exertional Malaise. Journal of Chronic Fatigue Syndrome, 14(2): 77-85. http://www.tandfonline.com/doi/abs/10.1300/J092v14n02_07
Samuel P. Watson, Amy S. Ruskin, Valerie Simonis, Leonard A. Jason, Madison Sunnquist, and Jacob D. Furst, “Identifying Defining Aspects of Chronic Fatigue Syndrome via Unsupervised Machine Learning and Feature Selection,” International Journal of Machine Learning and Computing vol.4, no. 2, pp. 133-138, 2014. http://www.ijmlc.org/index.php?m=content&c=index&a=show&catid=44&id=438
What Having M.E. Is Really Like. Meg Says (blog). http://www.meg-says.com/2015/12/what-having-me-is-really-like.html#.VpPV-0qAOko