ANZMES (the National Advisory on ME/CFS and a RNZCGP registered provider of continuing education) has released a short reference guide for secondary care. The resource acts as a guide for healthcare professionals in managing hospital stays for patients suffering from severe-very severe Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and long COVID (lC). It aims to improve patient care by addressing the unique needs and symptoms of patients with severe ME/CFS and lC during their hospital admissions.
“ME/CFS is a complex condition and its severity is often misunderstood by healthcare professionals. Severe patients are housebound. Very severe patients are bedbound, with very high needs requiring 24/7 care. Hospitalisation often occurs due to undernutrition, infections, and dysautonomic issues. Therefore, it is crucial that healthcare professionals have the knowledge to effectively manage patients during hospital admissions so as not to exacerbate their severe and debilitating symptoms,” says ANZMES president, Fiona Charlton.
“Our aim with this new resource is to provide a clear and concise reference guide for healthcare professionals to enhance patient care. While the assessment and evaluation of long COVID may differ from ME/CFS, the management of long COVID closely mirrors it, so we have leveraged our medical team’s expertise to develop a guide to support the effective care of these patients in a hospital setting.” She says.
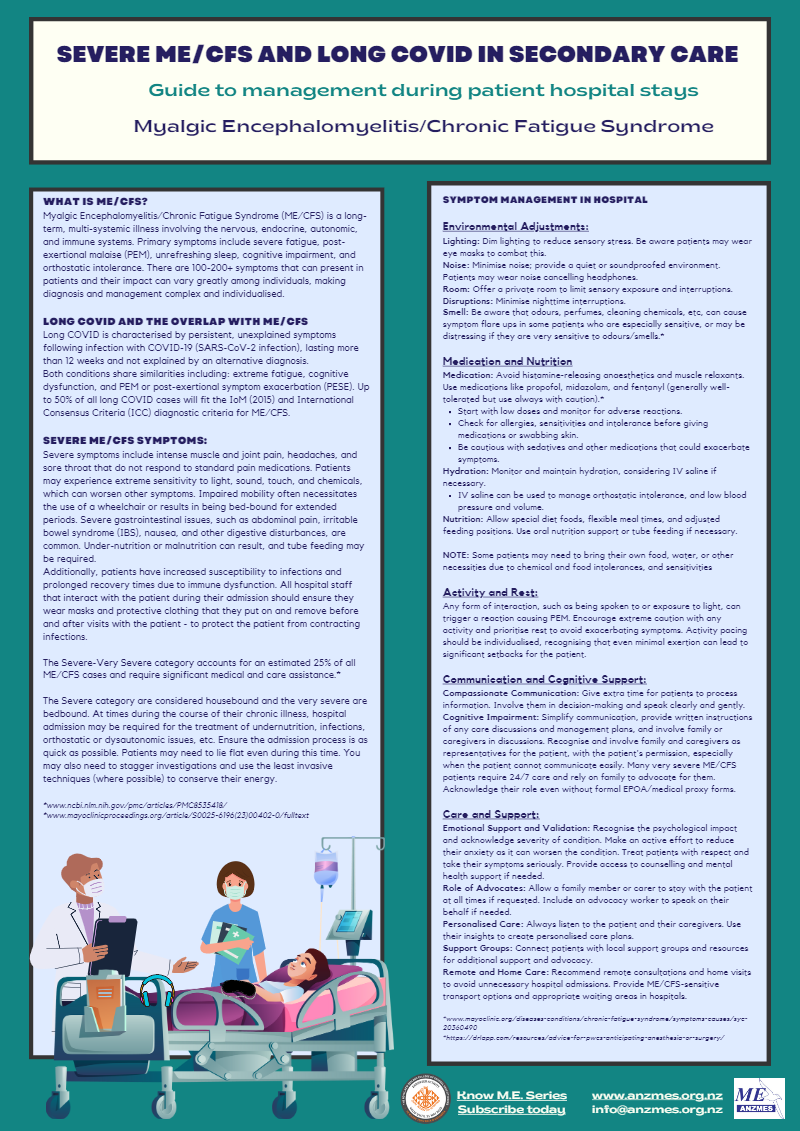
The resource outlines essential strategies for managing severe symptoms, including intense muscle and joint pain, extreme sensitivity to light, sound, touch, and chemicals, impaired mobility often necessitating a wheelchair, severe gastrointestinal issues, and increased susceptibility to infections due to immune dysfunction.
“For very severe patients, a light touch of the arm can be interpreted by the body as pain. Bright light can cause post-exertional malaise. People with very severe ME/CFS and long COVID spend the majority of their lives in darkened rooms, wearing noise cancelling headphones and eye masks. They are unable to eat properly, or bathe and toilet themselves without full time carers, and it is often a family member who assumes this role.” The impact of this on everyone cannot be underestimated.
An overview of key recommendations include:
- Sensory Adjustments: Dim lighting, minimise noise, and provide private rooms to reduce sensory stress.
- Medication and Nutrition: Avoid histamine-releasing anaesthetics and muscle relaxants. Use medications like propofol, midazolam, and fentanyl with caution. Monitor hydration and consider IV saline for orthostatic intolerance.[1]
- Activity and Rest: Recognise that even minimal interactions, such as being spoken to or exposure to light, can trigger PEM. Prioritise rest and avoid any unnecessary activity.
- Communication and Cognitive Support: Involve family and caregivers as representatives, especially when the patient cannot communicate; or simplify communication by providing written instructions and allowing extra time for patients to process information.
- Care and Support: Recognise the psychological impact, validate the severity of conditions, and provide access to counselling and mental health support. Include family members or caregivers in discussions and allow them to stay with the patient if requested.
ANZMES emphasises the importance of personalised care plans, the involvement of patient’s family members and their regular health team to understand the severity of their condition. The guide also encourages connections with local support groups and resources for additional advocacy and support for not only patients, but also their carers to avoid burnout. Remote consultations and home visits are recommended to avoid unnecessary hospital admissions.
ANZMES president, Fiona Charlton concludes “We believe that education is key to improving outcomes for patients with severe-very severe ME/CFS and long COVID. By providing this resource, we aim to enhance the knowledge and confidence of healthcare professionals so they are equipped when these patients are admitted under their care.”
Understanding ME/CFS and long COVID:
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a long-term, multi-systemic illness affecting the nervous, endocrine, autonomic, and immune systems. Patients experience severe fatigue, post-exertional malaise (PEM), unrefreshing sleep, cognitive impairment, and orthostatic intolerance. With over 100-200+ potential symptoms, the condition’s impact can vary greatly, making diagnosis and management highly individualised. Roughly 25% of all ME/CFS cases are categorised as mild, 50% as moderate-severe and 25% as very severe.[2] [3]
Long COVID is characterised by persistent, unexplained symptoms following infection with COVID-19 (SARS-CoV-2) lasting more than 12 weeks and not explained by an alternative diagnosis. Both conditions share symptoms such as extreme fatigue, cognitive dysfunction, and post-exertional symptom exacerbation (PESE), with up to 50% of long COVID cases fitting the diagnostic criteria for ME/CFS.
Post-Exertional Malaise (PEM)
Post-Exertional Malaise (PEM), also referred to as post-exertional symptom exacerbation (PESE) in the context of long COVID, is a debilitating response to normal, every-day activities in people with ME/CFS. For individuals with severe-very severe ME/CFS or lC, this can be triggered by sensory overload, such as exposure to light or even simple conversations. Repeated episodes of PEM can exacerbate these already severe symptoms, and even minimal exertion can lead to significant setbacks for the patient’s health and wellbeing.
About ANZMES
ANZMES, the Associated New Zealand ME Society, is the National Advisory on ME/CFS. Established in 1980, ANZMES has been at the forefront of research, representation, and education for ME/CFS in Aotearoa/New Zealand. The organisation is a registered provider of continuing medical education with the Royal New Zealand College of General Practitioners (RNZCGP) and is dedicated to improving the lives of those affected by ME/CFS and long COVID. ANZMES is a founding member of the World ME Alliance.