I was deeply saddened to learn that Dr. Paul Cheney had passed away on June 10th. Along with Dr. Dan Peterson, Dr. Cheney practiced in Incline Village, Nevada during the outbreak of what appeared to be a new disease. It had the hallmarks of a viral infection, but their patients were not recovering. That disease would later be called “Chronic Fatigue Syndrome.”
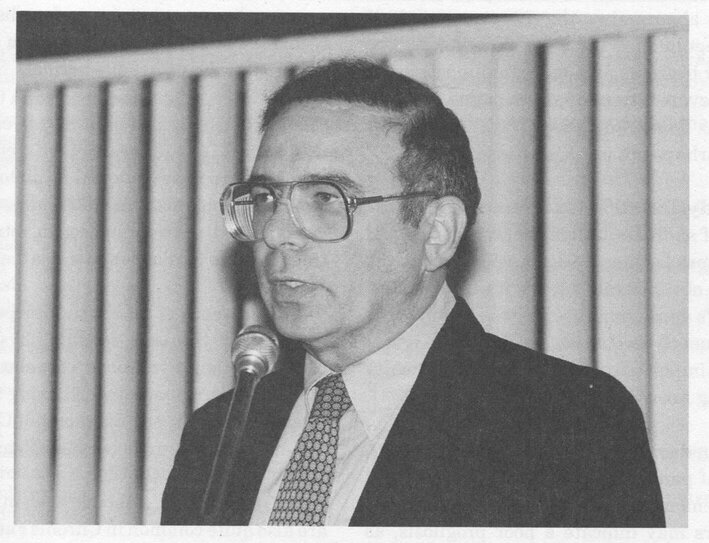
Dr. Cheney’s passing has personal significance for me, because he was the doctor who diagnosed me in 1993. I had heard about him through the leader of our support group in Austin, Texas, who generously allowed me to listen to a tape she had made of her consult with him. I was impressed with Dr. Cheney’s wealth of knowledge, which stemmed not just from his clinical practice, but from his research background in immunology. He not only had an MD, but held a PhD in physics and had been a research associate in the Division of Immunology at the CDC. He had also served as Chief of Medicine at the USAF Hospital in Mt. Home, Idaho for three years before going into private practice.
On the wall of Dr. Cheney’s office was a map with pushpins indicating where his patients came from. There were pushpins in every state and all over the world. Over the course of his practice he saw thousands of patients, whom he tested extensively for immune and metabolic dysfunctions, cardiac function, co-infections (including Lyme disease), indicators of viral reactivation, antigen sensitivity, and autoimmune activity, among others. I don’t think anyone understood ME/CFS as well as he did. Dr. Cheney was our “resident genius.”
Dr. Cheney spent four hours with me during our initial consult. He was not just thorough, he was kind. When he pronounced me “severely ill” there was genuine concern in his eyes. He gave me a piece of advice that I never forgot. “You are in a leaky boat,” he said. “How much can you throw overboard?” Throwing things overboard has saved me on many occasions.
The last time I saw Dr. Cheney was at the IACFS/ME Conference in San Francisco in 2014. I gave him a big hug and introduced myself as a former patient. “I remember you,” he said. It had been 21 years.
RIP Dr. Cheney. The world is poorer without you in it.
More information
Dr Cheney on heart function – from Dr. Myhill’s site: “Dr Paul Cheney has been working with the CFS patients clinically and experimentally for decades and this page is based on many of his ideas. This pulls together many clinical issues which hitherto were inexplicable to me and provides the basis for new therapies for CFS.”
Phoenix Rising Dr. Cheney page – Contains many links to protocols, treatment plans, etc. Some links are dead, but most are still active.
The Cheney Chronicles #2: His Protocol For Chronic Fatigue Syndrome – Cort Johnson’s blog, Health Rising, has two articles detailing one patient’s consult with Dr. Cheney.
ProHealth has a number of articles about Dr. Cheney’s treatment approach.
A Colossus in the ME/CFS Field Passes: Remembering Paul Cheney MD, Ph.D. – Cort Johnson talks about the treatments Dr. Cheney used, as well as his theories about the pathophysiology of ME/CFS.